Our pelvic floor is often overlooked and dismissed. Which really does our body a disservice because it has a huge role in support, bladder function, bowel function and sexual function. Due to the private nature of its function, many patients (and even practitioners) don't ask questions about it. But the pelvic floor are muscles just like any other. Did you know there are three layers to the pelvic floor?
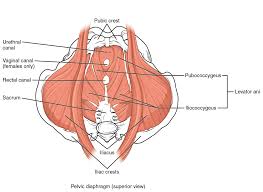
Pelvic Floor Muscles:
All of these muscles are often lumped together under the umbrella term of "pelvic floor". However they are each unique and have their own name!
- Layer 1: Ischiocavernosus, Bulbocavernosus/Bulbospongiosus (interchangeable), superficial transverse perineum, External Anal Spinchter
- Layer 2: Deep Transverse Perineum, Spinchter Urethrovaginalis (in patients with vaginas), External Urethral Spinchter
- Layer 3: AKA "Levator Ani" as a group; Puborectalis, Pubovaginalis (in patients with vaginas), Pubococcygeus, Iliococcygeus, Coccygeus
These muscles receive innervation from sacral nerve branches (S2-S4) and the pudendal nerve. The pudendal nerve has three branches: Inferior Anal Nerve, Perineal Nerve, Dorsal Nerve of the Penis/Clitoris. The pelvic floor attaches front to back and is positioned kind of like a hammock. It works closely with the diaphragm, the transverse abdominal muscle, and the multifidi muscles in our back to form our "core" of stability.
.jpg?width=159&height=343&name=close-up-of--a-white-beer-can-template-on-white-background-(1).jpg)
Soda Can Theory
Think of a soda can. If you pop the top on that can, it immediately is no longer firm and you can squish the contents around right? The same thing happens when any one of these areas isn't functioning properly. The pelvic floor is sensitive in nature and often not brought to the table when discussing problems. You could be walking around with your soda can open! The pelvic floor, like any other grouping of muscles can be tight, or too loose, weak or uncoordinated. It can sustain trauma and tears too. Childbirth, abuse, and pelvic surgeries (like a vaginal hysterectomy) are all examples of physical changes to the pelvic floor.
Pelvic Floor Dysfunction
What happens when the pelvic floor is tight or weak, uncoordinated etc? Breakdown. There are a variety of pelvic related dysfunctions that are related directly or indirectly to their function.
This isn't even an exhaustive list! The pelvic floor is involved in everything we do!
Treating Pelvic Floor Dysfunction
How do we go about treating the pelvic floor dysfunction? We start with an in depth evaluation where we discuss your pelvic history, symptoms, and goals. Then, we take a look at how the hips move and how strong they are. They attach onto the pelvis, just like the pelvic floor muscles. We want to make sure the pelvis is balanced, because if one side is slightly higher or rotated, it can be pulling on the pelvic floor muscles, not putting them in an optimal position. Next we assess the abdomen and your breathing! Remember that core? Good proper breathing is essential to that support! If the abdomen has restrictions (like from scars or just fascial hang ups) it can inhibit bladder and bowel function and of course pain! Finally we get around to checking the pelvic floor muscles externally and then internally if you're comfortable. Externally we would watch to see how the pelvic floor contracts and if it moves the perineum. We can also assess for redness, irritation and tenderness. Internally we can get a better assessment of the different layers of the pelvic floor and compare left to right. We are not gynecologists, we don't use speculums. Many of our patients have had terrible experiences with speculums, so fear not, its not part of our exam!
How to check pelvic floor
When we find muscles that are weaker and tight, we first start with releasing those muscles. Your therapist will use a single finger to continue to press on those muscles lightly to help stretch them. We may even add counter pressure around your hips and pelvis to further slacken those tissues and make it less tender. We are looking for your feedback during treatment and want you to be present with us. We will even teach you diaphragmatic breathing (also known as belly breathing) and how to relax your pelvic floor. This will help aid your therapist in further relaxing the pelvic floor.
Weak Pelvic Floor Muscles
Think of a closed fist. If it's closed, can you squeeze it closed any further? No. We want your pelvic floor to be able to contract AND relax so that it's able to do its job. When it's tight, like the closed fist, it's not able to do that and help prevent leaking, and support your body. If your pelvic floor is tight, our first step is to teach it how to relax and release the muscle(s). Once we have decreased the tightness and the pelvic floor is able to stay that way, and you are no longer having pain, we can start with strengthening.
Kegels
Have you heard of Kegels? Pelvic floor contractions are used interchangeably with the term kegels. There are different kinds of pelvic floor contractions! Similar to running, there are endurance holds (like a marathon), quick flicks (like sprints), and regular garden variety kegels.
During evaluation and treatment your therapist may find that different layers of the pelvic floor work better than others, or one side works better than the other. Sometimes we see that match up with hip weakness or tightness. Your therapist will use a variety of verbal cues with the tactile feedback from their finger to help you engage those muscles better.
Correct Kegels
"Imagine you are using your vagina to sip through a martini straw."
It's a silly imagery, but everyone knows what it's like to sip a drink through the tiny cocktail straws. That's the drawing up and in that we want the pelvic floor to do! Another one heard commonly is "draw up and in like you are trying to stop your flow of urine midstream."
This usually helps identify the muscles a patient needs to use, but the problem with it is, many patients will routinely practice stopping their flow of urine while on the toilet! This is a big no no! We don't want to do anything that disrupts the natural communication between the pelvic floor and the bladder. Doing that repeatedly could make it difficult for you to initiate your stream of urine (called hesitancy).
Once your therapist feels confident in your ability to perform a pelvic floor contraction properly they will likely give you homework to practice them! This is an area where less is more! Starting with the recommended number of kegels is important because it is entirely possible to fatigue out the pelvic floor, thus making urinary incontinence worse! Listen to your therapist when they tell you how many per day and how to space them out, it matters!
Physical Therapy for the Pelvic Floor
How do you know if you need pelvic floor physical therapy?
Do you have one or more of these symptoms:- Urgency: an intense sensation to empty the bowels or bladder, unrelated to the amount of urine or fecal material present
- Frequency: related to urgency, the number of times you are emptying the bladder or bowels
- Incontinence: the loss of control of the bowels or bladder, resulting in leaking
- Hesitancy: difficulty initiating stream of urine
- Incomplete emptying: feeling like there is residual amounts of urine or fecal material left after emptying
- Nocturia: getting up overnight to go to the bathroom (1x per night is typical)
- Dysuria: pain with urination
- Pelvic Pain: pain in the vulva, penis, testicles, perineum, bladder, lower abdomen, groin
- Pain with intercourse: pain at any point during sex, pain with orgasm/ejaculation
- Constipation: difficulty passing hard bowel movement, requiring straining
- Scars: from abdominal or pelvic surgeries
- Pelvic organ prolapse: dropping of pelvic organs caused by loss of support of the vagina
These are common symptoms we see related to pelvic floor dysfunction and can accompany any number of pelvic floor related issues. lease understand this is not an exhaustive list! You may realize you have some of these symptoms, and had just accepted them as your normal long ago. Plenty of the patients we see have a chronicity to their pelvic dysfunctions. That doesn't mean they can't be helped by physical therapy! Pelvic floor physical therapists do extensive continuing education in order to threat the pelvic floor. Not every therapist is equipped to treat such a sensitive and personal area. Still not sure? Chances are, if you think you might need pelvic floor physical therapy, you do. You know your body better than anyone else.
Pelvic Floor PT while Pregnant?
Pelvic floor therapists are also uniquely trained to treat patients who are pregnant. Even if you have a problem that you think is not related to the pelvic floor. The body undergoes a lot of changes during pregnancy and we can help ease/support some of those changes.
Common things we hear related to pelvic floor physical therapy:
"I'm just having back/hip/SI pain, that's not my pelvic floor!
You're correct. That isn't your pelvic floor. When we treat the body, regardless of the area, we zoom in and zoom out on the surrounding structures. There are fascial connections all through our body that can have huge implications.
For example there is one layer of fascia above the belly button, and two below it. The fascial connections below the belly button actually continue into the second layer of the pelvic floor! WOAH. The adductors (muscles on the inside of the thigh) will refer pain up into the pelvic floor and abdomen.
It's imperative to look at the whole picture. Due to the proximity of the pelvic floor to the LB, hips and SI joint, there can be an unresolved issue in the pelvic floor that is slowing down recovery in one of those areas.
You are always in control of your treatment, but if your therapist makes a recommendation to evaluate the pelvic floor, at least give it some thought! It could be the reason you finally kick low back pain to the curb!
"I'm really strong and work out all the time, my pelvic floor can't possibly be weak!
Therapists see this time and time again. Muscle imbalances happen everywhere in the body; the pelvic floor is no different. Part of the reason you are struggling with your squat can be related to pelvic floor needs! Don't forget to include the pelvic floor in your work outs! A simple way to do this is engage the pelvic floor (once your therapist has taught you how of course) during your work outs. You might be surprised at the extra power and endurance you have. That's because everything in that soda can is functioning together as you should!
Physical therapy for the pelvic floor in Columbia and Baltimore, Maryland
Your pelvic floor is a unique and sensitive area that deserves attention! Improving it's function can have a huge role in pelvic healthiness. If you want to know more about pelvic floor physical therapy, and if it's right for you, contact us today!